LATEST NEWS
Now Accepting Credit Cards
Great News! Now Accepting Credit Card Payments
We’re making it easier than ever to manage your health-related payments. You can now pay for COBRA premiums, Member premiums, FSA reimbursements, and more using your credit card!
✔ Convenient
✔ Secure
✔ Fast Processing
Take advantage of this new payment option today—because your time and peace of mind matter.
Contact us at (228)865-0514 to learn more!
Visit FSA Store now!
SAS is happy to announce that we have partnered with Health-E Commerce (FSA Store) in order to give our members more options for spending their Flexible Spending funds.
When you order through FSA Store, all purchases are 100% eligible and automatically substantiated! Note: Affiliate partners such as the Optical Shop or Oura Ring may require a receipt.
FSA Store takes the guess-work out of which services are FSA-eligible products including newly eligible over-the-counter medicines and menstrual care products!
- Exclusively stocked with eligible products
- Products Sourced Directly from Manufacturer
- No receipts necessary IIAS Merchant!
- Competitive pricing and Insiders deals
- 24/7 customer service specialists - FCS certified agents
- Free shipping on orders $50+
Visit FSA Store now to get started!
Select Administrative Services has MOVED!
Our new office is located on the Third Floor of the North Court One Building at 2304 19th Street, Suite 300, Gulfport MS 39501.
Members can now receive payments faster using direct deposit!
Great news! Select Administrative Servicess has partnered with Zelis Payments so you can quickly and easily receive reimbursements direct to your bank account using direct deposit. To enroll with Zelis Payments’ member direct deposit, please follow the registration instructions below.
Why should you enroll in Zelis Payments direct deposit?
- Receive payments faster – no need to wait 7-10 days for a check in the mail. You’ll get paid within 1-2 business days of receiving a payment notification.
- No transaction fees – all fees associated with direct deposit are covered courtesy of Select Administrative Services.
- Manage payment and banking records instantly – gain immediate access online to view previous payments, explanation of payment (EOP), manage banking information and to set up customized notifications.
Enrolling is fast and easy! Visit member.zelispayments.com and click “Sign-Up Now!” to create an account. Follow the instructions below as a guide:
1 - Request your registration code
- Click the “I don’t have a Registration Code” link on the enrollment page.
- Complete the required fields with your contact information and select how you would like to receive your code.
- Click “Request Registration Code”.
- Once you have received a code via phone or email make sure to follow the rest of the instructions below.
2 - Enter your registration code
- Enter your registration code and your email address.
- Ensure that all other fields have been filled in, select your username and click “Register.”
3 - Create a password
- Once you’ve clicked “Register” you will receive an automated email with a link to create your password.
- After adding your password, you will be redirected to a log in screen. From here you can access your new account.
4 - After logging in, select Virtual Reimbursement Account (VRA) Direct
- Your user account is now active! Make sure to select VRA Direct to complete adding direct deposit.
- Once you’ve completed your bank setup, Zelis will initiate a pre-note test on the account provided for additional security verification. A small deposit will be made in a random amount no larger than $1.00.
- Review your bank statement for the deposit and log-in to the Zelis portal to enter the exact amount for final confirmation.
That's it! Now you can start receiving payments from Select Administrative Services through direct deposit. All payment information is available 24/7 via the Zelis Payments Member Portal and can be downloaded to PDF. For any additional information or questions please call the Zelis Payments Client Service department at 1-800-536-9042.
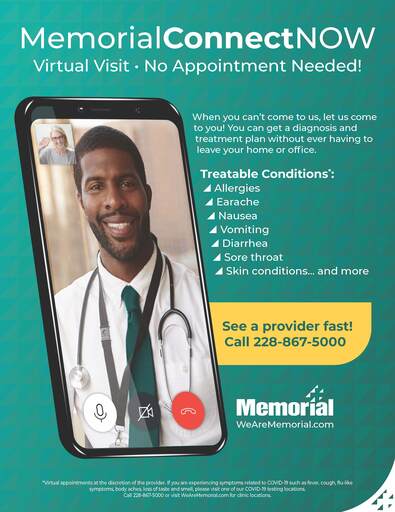
MemorialConnectNOW
Virtual Visit - No Appointment Needed!
New Web Portal - VBA Gateway
Register for our new Web Portal VBA Gateway.
Members
You should receive a letter with your Registration Code in the mail. If you do not receive this or need any assistance getting registered, please contact SAS Customer Service.
Providers
Please navigate to https://sas.vbagateway.com/. Choose Click here to register and/or enroll. Choose Provider Portal to register.
Please contact SAS Customer Service for assistance at 228.865.0514.
Members, You can now View and Print your ID Card online!
Log into your Gateway Member Account today to see this new feature for SAS members.
- Click on the View/Print ID Card tab.
- You can either Print or Download a copy of the card to your computer or phone.
New Coordination of Benefits E-Form Available
You can now complete and submit your annual Coordination of Benefits form online through your member account in Gateway.
- Click on the Create a Request tab.
- Click on Upload Document.
- Click on the Fillable COB Form.
- Fill out the form and download it to your computer.
- Once you have filled out and saved your PDF form, click the NEXT button below to proceed to form submission.
- Click Upload My File and select the file you just completed.